Unfucking Progesterone and Estrogen in Perimenopause
Demystifying HRT, hormones, and ways to NOT feel like shit in perimenopause.
Did you know that perimenopause isn’t just chaotic hormone fluctuations, but a sequence of perfectly normal events — much like puberty? It begins in your late 30s to early 40s with declining progesterone paired with high, wildly fluctuating estrogen, and ends with low progesterone and low estrogen at menopause.
If you’re feeling overwhelmed with symptoms such as anxiety, breast pain, hot flushes, sleep disturbance, hair loss, brain fog, migraines, and heavy periods (perhaps some or all of the above), understanding perimenopause and the underlying changes in progesterone and estrogen is vital in terms of determining the next steps forward.
Knowing more about perimenopause can empower us to make important lifestyle changes and equip us to have productive conversations with our doctors and endocrinologists. This can help us move through perimenopause feeling healthier and more confident, rather than suffering for many years until menopause finally arrives.
Progesterone benefits
During perimenopause our progesterone levels slowly decline, while estrogen fluctuates wildly and is often very high. Losing progesterone can result in memory loss, anxiety, sleep disturbance, hot flushes, hair loss, heart palpitations, heavy periods and an increased risk of depression1.
Progesterone is good for mood, sleep, and healthy thyroid function. Progesterone also has a natural inhibitor of 5-alpha-reductase, an enzyme that converts testosterone into DHT, which means that progesterone stimulates hair growth and has anti-androgen properties. Progesterone stabilizes the HPA (adrenal) axis, and can even reduce the risk of breast cancer.
Testing progesterone levels
The best time to test your progesterone levels via a blood test is when you’re at the “peak progesterone” phase of your cycle, which is 7 days before your period (Some naturopaths will say “day 21”, but this is only correct for people who have a 28 day cycle).
With a 21-day cycle, test progesterone on approximately day 14
With a 28-day cycle, test progesterone on approximately day 21
With a 35-day cycle, test progesterone on approximately day 282
When your results come back, you’ll be comparing your results with the mid-luteal reference range (sometimes called the “intermediate luteal” range). According to Naturopathic Doctor Lara Briden, author of the Hormone Repair Manual, the optimal range of peak progesterone is greater than 8 ng/mL (25 nmol/L), and if it’s less than 4 ng/mL (13 nmol/L) you didn’t ovulate.
Increasing progesterone
To make more progesterone naturally, Lara Briden, explains that “the only way to make progesterone is to consistently ovulate every month.” To do that, we need to support overall general health by reducing stress, correcting any underlying inflammation issues, reversing insulin resistance, and supporting the thyroid.
In addition to improving overall health to support ovulation, you may decide to take oral micronised progesterone (brand names: Prometrium, Teva, Utrogestan, Famenita). Dr. Jerilynn Prior, an MD and Professor of Endocrinology and Metabolism at the University of British Columbia in Vancouver (she’s basically a pioneer in women’s health), states that progesterone alone, rather than progesterone plus estrogen, is usually the best choice of hormone therapy for perimenopause.3
Dosage for progesterone capsules start at 100 mg to 300 mg. Progesterone cream is a lower dose alternative and is available over-the-counter in Australia, but at only 20 mg per pump it may only work for mild symptoms. Usually, you take the tablets or apply the cream every evening for the last 14 days of your cycle.
This double-blind, randomized trial of 300 mg oral micronised progesterone found a significant improvement in night sweats and sleep quality in perimenopausal women.
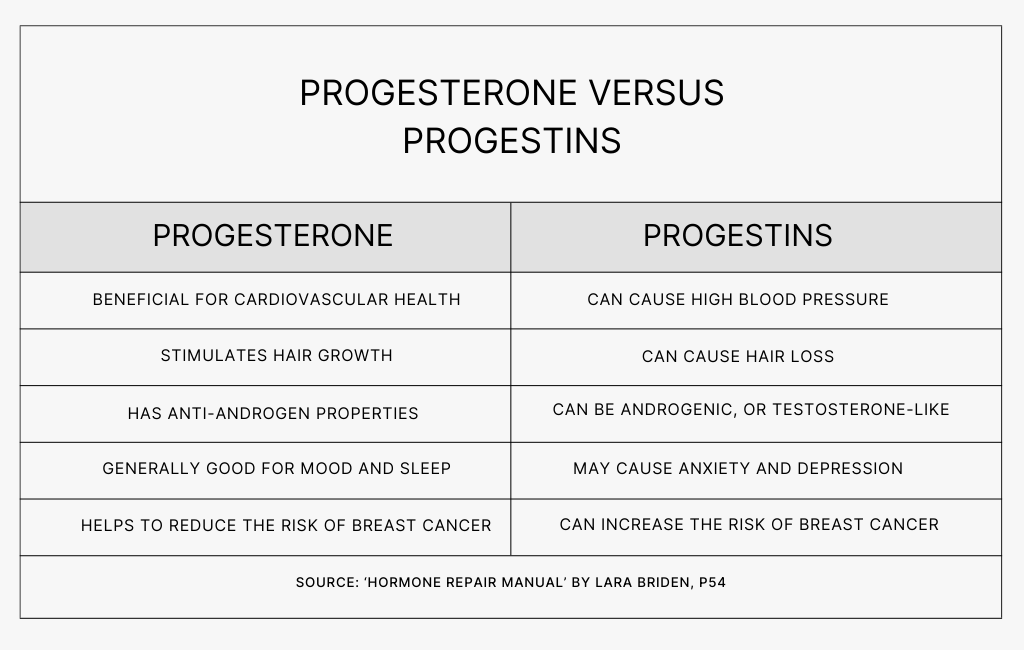
Progesterone vs progestins
You may have heard about the risks associated with progestins, which are still in contraceptive drugs like the pill (note that there is no progesterone in hormonal birth control), and were included in the old HRT4 that is still sometimes prescribed today.
Progesterone is very different to progestins; the terms cannot be used interchangeably and they often have the opposite effect. Furthermore, oral micronised progesterone and progesterone creams do not carry a clotting risk like oral estrogen and some progestins.
What about estrogen?
Together with progesterone, estrogen helps build muscle and bone, plus maintain the health of the brain and heart, and is important for maintaining a healthy metabolic rate by enhancing insulin sensitivity, which helps prevent insulin resistance and diabetes. Estrogen is often high (but fluctuating) during perimenopause, then low in menopause.
While progesterone alone is usually the best treatment during perimenopause, if hot flushes continue beyond the final period (i.e. in menopause5), they are the result of lower, but still fluctuating, estrogen. Lara Briden states that they can be improved with progesterone plus estrogen. Menopausal symptoms such as insomnia, memory loss and vaginal dryness can also respond to progesterone plus estrogen therapy6.
Lara Briden states that no menopausal woman should need more than 50 mcg of estrogen, and recommends that menopausal women start with progesterone, then add 25 mcg of estradiol if needed, going up to 50 mcg only if they still have symptoms7. Sometimes women in early menopause will find that they’re still having estrogen spikes and will need to lower their dose, or go back to progesterone only8.
Dr. Prior is an advocate for progesterone-only therapy for both perimenopause a menopause, but states that if you decide to take estrogen in menopause, you should also take progesterone — even if you don’t have a uterus9.
Modern estrogen therapy is usually bioidentical estradiol absorbed through the skin, which allows it to directly enter the bloodstream and not form dangerous blood-clotting factors in the liver. The safest type of estrogen is an estradiol patch (Estradot or Climara), gel (Sandrena or Estrogel). The Estradot patch comes in strengths of 25 mcg to 100 mcg.
Estrogen therapy is associated with a small increase in breast cancer risk of 0.1%, which is similar to the risk from alcohol or low physical activity10. However those statistics are based mostly on data about non-body identical hormones such as Premarin, which is a conjugated equine estrogen11.
Testing Estrogen Levels
Because perimenopause leads to a roller coaster of extremely high spikes of estrogen combined with regular drops, testing estrogen levels during perimenopause is unlikely to provide useful information. Naturopaths, please don’t come at me.
If you really wanted to test, then you’ll probably need to check your estrogen a few times. Many naturopathic doctors recommend a DUTCH test from urine samples as the most accurate method — it’s up to you whether you feel that’s necessary.
If you do blood tests, according to Lara Briden: Early in the cycle (day 2 or 3), estradiol should be very low, typically below 50 pg/mL (180 pmol/L). A few days before ovulation (around day 10 of a 28-day ovulatory cycle), peak estradiol should be 200 to 400 pg/mL (700 to 1400 pmol/L).
Magnesium & Taurine
A 2017 paper, “Magnesium in the gynecological practice: a literature review,” found that magnesium is an effective treatment for the symptoms of menopause and perimenopause and works by “normalizing the action of hormones (mainly progesterone) on the central nervous system.”
Magnesium also supports the thyroid, calms the nervous system, regulates the HPA axis, reduces blood sugar, helps to normalise insulin, and is anti-inflammatory. Lara Briden says to opt for magnesium glycinate, bisglycinate, or threonate. Skip the magnesium oxide; a 2019 study found it had the lowest bioavailability.
According to Lara Briden, magnesium could be as much treatment as you need for mood, sleep, and hot flashes. She suggests people try it for a few weeks, and then look at adding progesterone as the next step.
Taurine supplementation may also help balance out estrogen in perimenopause since it supports healthy estrogen metabolism or detoxification, however it may not be a good choice for people who suffer from psoriasis. Psoriatic lesions also contain elevated amounts of taurine, according to 2016 research.
Perimenopause, Menopause & Insulin Resistance
When it comes to perimenopause and menopause, insulin resistance is a key consideration because it can worsen almost any symptom12. Lara Briden states that healthy fasting insulin should be less than 10 mIU/L (60 pmol/L), which is already a lot lower than standard lab ranges. She also states that “it’s probably not possible to lose much abdominal weight, or abdominal fat, until fasting insulin comes below 8 mIU/L”.
Reversing insulin resistance involves eating more whole foods, avoiding sweet drinks, reducing processed carbs, supplementing magnesium, maintaining a healthy circadian rhythm (go to bed on time and get morning sunshine), and moving more. An interesting 2022 meta study in the Sports Medicine journal found that light-intensity walking in short 2 - 5 minute bursts significantly improved insulin levels after meals compared to prolonged sitting and standing breaks.
A Word on HRT
A lot of the fear around Hormone Replacement Therapy (HRT) is due to The Women's Health Initiative Memory Study in 2003 which looked at estrogen plus progestin therapy and found that it increased older women's risk for probable dementia. However as mentioned above, bio identical progesterone is completely different to progestins. The study also used conjugated horse estrogens rather than bioidentical estradiol.
Note that even though I refer to conjugated equine estrogens (CEE) and progestins as “old HRT”, they are still used today, particularly in birth control and in hormone therapy for postmenopausal women. If you’re unsure what you’re being prescribed, go to this useful table: List of bioidentical versus non-bioidentical hormone therapy.
When reading about HRT, make sure you check exactly which type of HRT you’re reading about. Conflating old HRT (CEE and progestin) with modern hormone therapy such as micronised oral progesterone alone, or micronised oral progesterone plus bioidentical estrogen, can lead to a lot of mixed information.
Resources:
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden. This book is well-written and jam-packed with important information about both perimenopause and menopause.
Estrogen’s Storm Season: Stories of Perimenopause by Dr Jerilynn Prior, a professor of endocrinology and a pioneer in women’s health. This book uses fictional case studies to share important facts about perimenopause. I personally didn’t like the story-telling approach and felt that it slowed down the information flow. I’m including it here because some people may prefer it over a textbook-style approach.
Dr Jerilynn Prior is also the founder and scientific director of The Centre for Menstrual Cycle and Ovulation Research (CeMCOR), which is an excellent resource for those of us who want our information to be more direct.
HRT, Breast Cancer Risk & Vaginal Estrogen: Risks & Myths Explained, with Dr. Corinne Menn is an interesting podcast with a slightly different view that’s worth considering. Dr. Corinne Menn shares her perspective as both a board-certified OB-GYN and 20-year breast cancer survivor. She states that while it’s correct that bio-identical progesterone and bioidentical estrogen are better than synthetic progestins and conjugated equine estrogens (CEE), the results of the Women’s Health Initiative study were exaggerated, and if some women need to take the “old HRT” they shouldn’t be afraid to do so. She also says that GPs, oncologists, and her fellow OB-GYNs aren’t taught a lot about menopause, so it’s vital that you become the “CEO of your own health”.
That’s it for now. Hopefully this information saves you a little bit of time and will lead to some important conversations with your health care providers. If you found this article useful, please click the heart down the bottom left of this page (it helps other people find my work). If you want to know more about me, click here.
Since perimenopause symptoms and underactive thyroid symptoms overlap, you may also like to read this article on fatigue, brain fog, hair loss and weight gain.
Please remember that you should always speak to your health professional before making any dietary or lifestyle changes; this is general information not specific to your situation.
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden
https://www.larabriden.com/right-way-test-progesterone/
Estrogen’s Storm Season, by Dr Jerilynn Prior.
“Old HRT” is progestins and conjugated equine estrogens.
If you’re in menopause, you’ll have an FSH level above 40 IU/L. However, if your FSH drops below 40 IU/L on a couple of occasions, then your lack of periods is not due to menopause but some other obstacle to ovulation. Source: Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden, page 56.
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden, page 16
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden
At a MenoClarity Live event, she explained: “Progesterone works with or counterbalances estrogen in every part of our bodies. Said another way, a woman who has had a hysterectomy (and thus has no uterus) still has breasts, brain, bones and heart that need progesterone.”
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden, page 142
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden, page 142
Hormone Repair Manual: Every woman’s guide to healthy hormones after 40, by Lara Briden, page 103.